Advancements in Understanding and Targeting Apolipoproteins in Alzheimer's Disease and Cardiovascular Disease (2020-2024)
Apolipoprotein Update: APOE & AD mechanisms/therapies, Lp(a)/ApoB & CVD risk/treatment, APOL1 & kidney disease insights.
Introduction
Apolipoproteins play crucial roles in lipid metabolism and have been implicated in the pathogenesis of both Alzheimer's disease (AD) and cardiovascular disease (CVD). This mini-review summarizes recent advancements (2020-2024) in understanding the roles of specific apolipoproteins, particularly APOE and lipoprotein(a) [Lp(a)], in these diseases, as well as therapeutic strategies targeting them.
APOE in Alzheimer's Disease: Mechanisms and Therapeutic Strategies
A significant body of research has focused on the role of apolipoprotein E (APOE) in Alzheimer's disease. The APOE4 allele is a well-established genetic risk factor for AD, while APOE2 appears to be protective.
Mechanistic Insights: Researchers have made significant strides in elucidating the mechanisms by which APOE isoforms influence AD pathology. Berislav V. Zloković's group at the University of Southern California demonstrated in 2020 that APOE4 contributes to blood-brain barrier dysfunction, predicting cognitive decline (Axel Montagne et al., 2020, Nature). Further work by Zloković's group in 2021 showed that APOE4 accelerates vascular and neurodegenerative disorders in Alzheimer's mice independently of amyloid-β via cyclophilin A (Axel Montagne et al., 2021, Nature Aging). David M. Holtzman's lab at Washington University in St. Louis has extensively studied the role of APOE in neuroinflammation. Their work in 2021 highlighted APOE-mediated neuroinflammation and neurodegeneration in AD (Samira Parhizkar et al., 2021, Seminars in Immunology). In 2022, Holtzman's group further demonstrated that selective reduction of astrocyte APOE3 and APOE4 significantly reduces amyloid-β accumulation and plaque-related pathology in a mouse model of amyloidosis (Thomas E. Mahan et al., 2022, Molecular Neurodegeneration). Chia-Chen Liu's research group at Mayo Clinic has also contributed significantly to understanding APOE's role. In 2022, they showed that peripheral APOE4 enhances Alzheimer's pathology and impairs cognition by compromising cerebrovascular function (Chia‐Chen Liu et al., 2022, Nature Neuroscience). This group's work in 2023 revealed cell-autonomous effects of APOE4 in restricting microglial response in brain homeostasis and AD (Chia‐Chen Liu et al., 2023, Nature Immunology). Yadong Huang's group at the University of California, San Francisco, demonstrated in 2023 that neuronal APOE4 removal protects against tau-mediated gliosis, neurodegeneration, and myelin deficits (Nicole Koutsodendris et al., 2023, Nature Aging). In 2024, Tony Wyss-Coray's group at Stanford University showed that APOE4/4 is linked to damaging lipid droplets in Alzheimer's disease microglia (Michael S. Haney et al., 2024, Nature).
Therapeutic Implications: These mechanistic insights have fueled the development of therapeutic strategies targeting APOE. Paramita Chakrabarty's group at Mayo Clinic Jacksonville reviewed therapeutic approaches targeting APOE function in AD in 2020 (Tosha Williams et al., 2020, Molecular Neurodegeneration). Rasha N.M. Saleh's group at University College London found in 2023 that hormone replacement therapy is associated with improved cognition and larger brain volumes in at-risk APOE4 women (Rasha N.M. Saleh et al., 2023, Alzheimer's res. ther.).
Apolipoproteins and Cardiovascular Disease: Risk Assessment and Therapeutic Interventions
Research on apolipoproteins in CVD has focused on risk assessment using apolipoprotein levels and therapeutic interventions targeting specific apolipoproteins.
Risk Assessment: Several studies have investigated the association between apolipoproteins and CVD risk. Nicholas Marston's group at Brigham and Women's Hospital found in 2020 that apolipoprotein B-containing lipoproteins are associated with an increased risk of myocardial infarction (Nicholas Marston et al., 2020, JAMA Cardiology). Jennifer Behbodikhah's group at Icahn School of Medicine at Mount Sinai reviewed apolipoprotein B as a biomarker and potential therapeutic target in CVD in 2020 (Jennifer Behbodikhah et al., 2020, Metabolites). Gissette Reyes-Soffer's group at Columbia University Irving Medical Center published a scientific statement from the American Heart Association in 2020, emphasizing lipoprotein(a) [Lp(a)] as a genetically determined, causal, and prevalent risk factor for atherosclerotic CVD (Gissette Reyes‐Soffer et al., 2020, Arteriosclerosis Thrombosis and Vascular Biology). John H. Contois's group at Vanderbilt University Medical Center discussed the standardization of Apolipoprotein B, LDL‐Cholesterol, and Non‐HDL‐Cholesterol in 2023 (John H. Contois et al., 2023, Journal of the American Heart Association). L. Renee Ruhaak's group at University of California, Davis, developed an LC-MRM-MS-Based Candidate Reference Measurement Procedure for Standardization of Serum Apolipoprotein (a) Tests in 2023 (L. Renee Ruhaak et al., 2023, Clinical Chemistry).
Therapeutic Interventions: Several studies have evaluated the efficacy of therapeutic interventions targeting apolipoproteins. Michelle L. O'Donoghue's group at Brigham and Women's Hospital investigated the long-term effects of evolocumab, a PCSK9 inhibitor, in patients with established atherosclerotic CVD (Michelle L. O’Donoghue et al., 2020, Circulation). Lorenz Räber's group at Bern University Hospital, Switzerland, showed that alirocumab, another PCSK9 inhibitor, added to high-intensity statin therapy, reduces coronary atherosclerosis in patients with acute myocardial infarction (Lorenz Räber et al., 2021, JAMA). Steven E. Nissen's group at Cleveland Clinic investigated the effect of short interfering RNA targeting lipoprotein(a) production (Steven E. Nissen et al., 2021, JAMA). Stephen J. Nicholls's group at Monash University evaluated the lipid-lowering effects of the CETP inhibitor obicetrapib in combination with high-intensity statins (Stephen J. Nicholls et al., 2022, Nature Medicine). Nicholls's group also reported on muvalaplin, an oral small molecule inhibitor of lipoprotein(a) formation (Stephen J. Nicholls et al., 2022, JAMA). Christie M. Ballantyne's group at Baylor College of Medicine evaluated obicetrapib plus ezetimibe as an adjunct to high-intensity statin therapy (Christie M. Ballantyne et al., 2023, Journal of clinical lipidology). Daniel Gaudet's group at Université de Montréal investigated plozasiran, an RNA interference agent targeting APOC3, for mixed hyperlipidemia (Christie M. Ballantyne et al., 2024, New England Journal of Medicine) and for managing persistent chylomicronemia and pancreatitis risk (Gerald F. Watts et al., 2024, New England Journal of Medicine). Robert A. Harrington's group at Stanford University investigated Apolipoprotein A1 Infusions and Cardiovascular Outcomes after Acute Myocardial Infarction (C. Michael Gibson et al., 2024, New England Journal of Medicine).
APOL1 in Kidney Disease
Recent research has also focused on the role of apolipoprotein L1 (APOL1) in kidney disease. Glenn M. Chertow's group at Stanford University investigated inaxaplin for proteinuric kidney disease in persons with two APOL1 variants (Ogo Egbuna et al., 2022, New England Journal of Medicine). Adriana M. Hung's group at Vanderbilt University Medical Center showed that genetic inhibition of APOL1 pore-forming function prevents APOL1-mediated kidney disease (Adriana M. Hung et al., 2023, Journal of the American Society of Nephrology). Opeyemi A. Olabisi's group at Washington University in St. Louis demonstrated that APOL1-mediated monovalent cation transport contributes to APOL1-mediated podocytopathy in kidney disease (Somenath Datta et al., 2024, Journal of Clinical Investigation). Suzie J. Scales's group at Genentech found that Apolipoprotein L1 (APOL1) renal risk variant-mediated podocyte cytotoxicity depends on African haplotype and surface expression (Nidhi Gupta et al., 2024, Sci. rep. (Nat. Publ. Group)).
Conclusion
Significant progress has been made in understanding the roles of apolipoproteins in AD, CVD, and kidney disease over the past five years. Mechanistic studies have provided valuable insights into how APOE isoforms contribute to AD pathology, paving the way for novel therapeutic strategies. In CVD, research has focused on improving risk assessment using apolipoprotein levels and evaluating the efficacy of therapeutic interventions targeting specific apolipoproteins, such as Lp(a) and APOC3. Studies on APOL1 have advanced our understanding of its role in kidney disease and potential therapeutic targets. These advancements highlight the importance of apolipoproteins as key players in human health and disease.
✨ About This POST
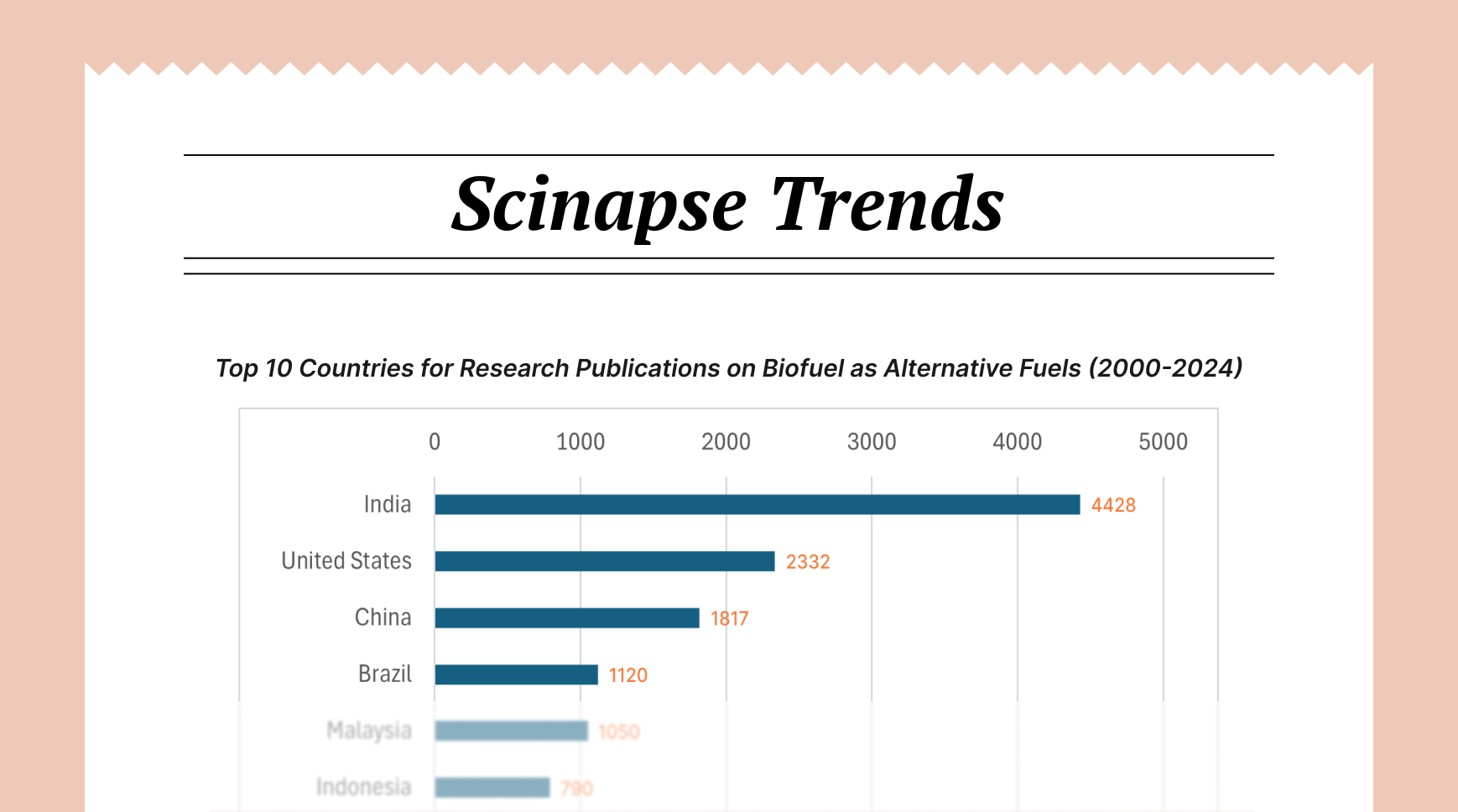
This mini-review post was generated through Scinapse. Scinapse provides reliable research trend analysis using citation analysis and AI technology.
Check out the trends in your field too!
Get started at https://scinapse.io

![[Global Research Trends] 10. Top 10 Countries on Microneedle Research Publications (2014-2024)](/content/images/size/w720/2024/11/Scinapse-Trends_10.png)
![[Global Research Trends] 9. Top 10 Countries on FOWT Research Publications and Authors' Normalized h-Index (2014-2024)](/content/images/size/w720/2024/11/Scinapse-Trends_9--1-.png)
![[Global Research Trends] 8. Leading Companies and Countries with Top Publications on Drug Approval Post-Covid (2021-2024)](/content/images/size/w720/2024/10/hand-medical-glove-holding-vaccine-vial-1.jpg)
Comments ()